What You Support
Trauma Care

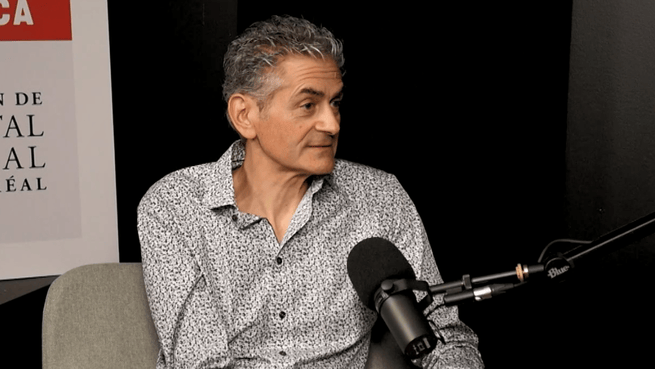
"The Dr. David S. Mulder Trauma Centre has the lowest mortality rate in the province. To maintain this exceptional performance, our team must stay at the top of its game and have access to cutting-edge technology. That’s why we need your support."
Chief of Trauma Services, MGH-MUHC
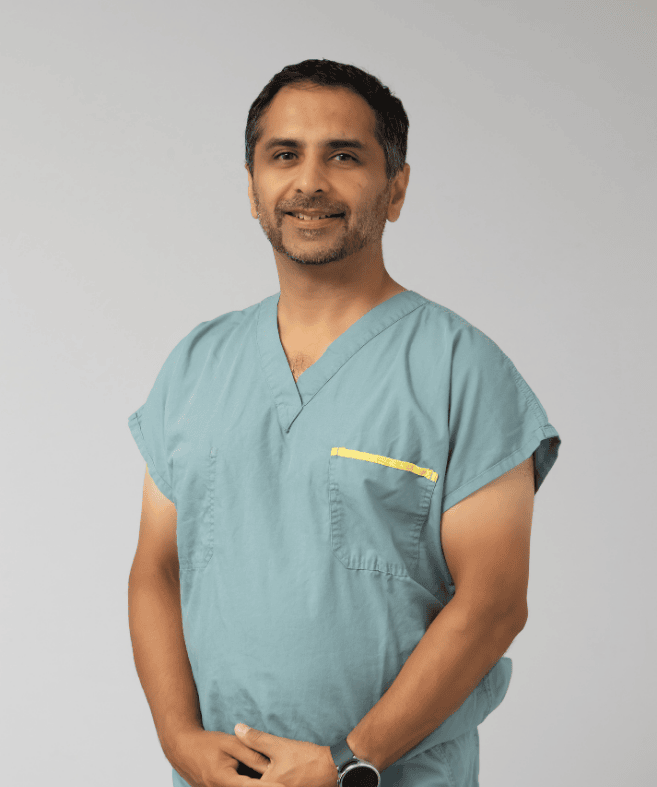
"Sometimes, you’re living a completely normal life, then suddenly, something happens that turns your life around. It’s really the medical teams that get you back on your feet. Otherwise, I know I either wouldn’t be alive, or I wouldn’t be living this life."
Grateful patient